Before We Begin — A Personal Note
Dear Caregiver,
If you’re here, it’s because you love someone with Down Syndrome and you’re looking for ways to help them live more comfortably and confidently. I understand the weight you carry — balancing medical appointments, therapies, daily routines, future plans, and the countless unseen tasks that fill each day.
That’s why I’m sharing this — because skin care can sometimes be a rare and beautiful “quick win” in our caregiving journey. And quick wins matter. In a role filled with long‑term, complex challenges that often demand endless patience, those moments when we can act and see a real change in days are like oxygen for the soul. They remind us that our efforts do lead to visible difference, and they give us the boost we need to keep going with hope and energy.
This information comes from the “Skin Conditions in Children and Adults with Down Syndrome” workshop I attended at the 2025 National Down Syndrome Congress (NDSC) Convention in Dallas, Texas, led by Dr. Jillian Rork, a dermatologist and pediatrician who specializes in caring for people with DS.
I am sharing what I learnt from her workshop in the hope that it will be helpful to you and your loved one — so that together, we can find and cherish those moments of comfort and relief, and build on them step by step.
Why People with Down Syndrome May Have More Skin Issues
Dr. Rork explained that certain skin problems appear more often — and may be more stubborn — in people with Down Syndrome because of:
- Differences in immunity – The immune system works differently, sometimes making it harder to fight off skin infections or calm inflammation.
- Differences in skin structure – The outer layer of the skin may not hold moisture as well as in others.
- Weaker “barrier function” – Think of the skin like a brick wall. The “bricks” are skin cells, and the “mortar” is natural fats and oils. In DS, the mortar can be weaker, which means water escapes more easily and germs or irritants can sneak in.
These differences mean that preventive skin care isn’t optional — it’s a simple, powerful way to improve daily comfort, prevent bigger problems, and boost confidence.
The “Big 6” Skin Concerns — and How to Help
Below are the six most common skin conditions Dr. Rork sees in her patients with DS. I’ve included what they look like, why they happen, and step‑by‑step tips for care — plus the exact products recommended at the workshop (and their active ingredients so you can find them wherever you live).
1. Dry Skin (Xerosis)
Looks like:
- Rough, bumpy, flaky, cracked, or peeling skin on the face and body
- Thickened skin on elbows, knees, or bottoms of the feet (hyperkeratosis)
- Light, dark, or pink patches of rough skin
- Itchiness, which can lead to scratching and open sores
Why it happens:
People with Down Syndrome often have a weaker skin barrier, which means water escapes more easily and irritants can get in. This is partly due to differences in skin proteins linked to the extra copy of chromosome 21. Weather, water exposure, detergents, medications, and family history can all make dryness worse.
Care tips:
- Moisturize at least twice a day — creams and ointments work better than lotions because they’re thicker and hold in moisture longer.
- Right after bathing, gently pat skin dry (don’t rub) and apply moisturizer immediately to lock in water.
- Choose products labeled fragrance‑free, hypoallergenic, and alcohol‑free.
- Short, lukewarm baths/showers (under 10 minutes) help prevent further dryness.
- Use mild, fragrance‑free cleansers only on dirty areas (armpits, groin, feet). Avoid bubble baths.
- Dress in loose, cotton clothing; avoid itchy fabrics or layer cotton underneath.
- Skip fabric softeners and dryer sheets; wear gloves outdoors in cold weather.
- Rinse and moisturize after swimming — pool chemicals can dry skin.
- Keep nails short to reduce scratching injuries.
- Use sun protection — mineral sunscreen or sun‑protective clothing.
Special note on hyperkeratosis (thickened skin):
- Common on palms, soles, elbows, and knees.
- Gentle exfoliation with a plain, fragrance‑free cleanser can help prevent buildup (ask your doctor how often).
- Moisturizers with urea, lactic acid, or salicylic acid can soften thick skin — but they may sting, so introduce slowly and watch for irritation.
- Comfortable, well‑fitting shoes help prevent thick skin on feet.
- Encourage alternatives to scratching (e.g., a “scratch‑dance” or hand squeeze) to protect skin.
Workshop‑recommended moisturizers:
- CeraVe® Moisturizing Cream — ceramides + hyaluronic acid
- Eucerin® Advanced Repair Cream — urea + ceramides
- Vanicream® Moisturizing Cream — gentle, fragrance‑free
- Aquaphor® Healing Ointment or pure petroleum jelly — for very dry spots
Sensory‑friendly application tips:
- Let your teen/adult choose between creams and ointments — creams are less sticky and may be more comfortable.
- Turn moisturizing into a game — draw shapes, letters, or favorite animals with the cream.
- Involve them in the process — even small steps build independence and ownership.
- Keep moisturizer visible and part of the daily routine (e.g., next to toothbrush or hand soap).
- Use a visual checklist to make moisturizing predictable and easy to remember.
When to call the doctor:
- No improvement after 2 weeks of consistent care
- Signs of infection (fever, pus, spreading redness)
- Painful cracks or very red skin
2. Seborrheic Dermatitis (Dandruff & Related Rashes)
Looks like:
- Flaky skin that may be dry, dusty, or greasy.
- Flakes can be white, yellow, or brown.
- Rash may look pink, lighter, or darker depending on skin tone.
- On the scalp: sometimes thick, stubborn build‑up that’s hard to clear.
- On the face: often in eyebrows, along the sides of the nose, cheeks, behind or inside the ears.
- Can also appear on the chest, upper back, armpits, belly button, or groin.
- May be itchy — but sometimes not itchy at all.
Why it happens:
Seborrheic dermatitis is very common in people with Down Syndrome, especially during the teen years, though it can appear at any age. It’s linked to overgrowth of a normal skin yeast (Malassezia) and changes in skin oil production. It’s not an infection, not contagious, and not caused by diet. Stress, cold weather, or illness can make it flare.
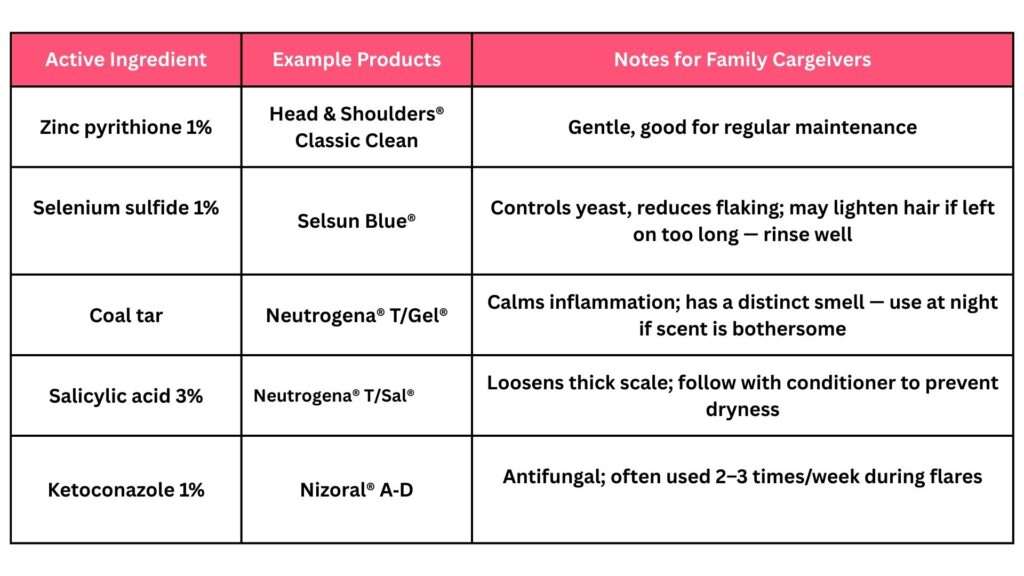
Care tips for scalp (dandruff):
- Use medicated dandruff shampoos directly on the scalp skin (not just the hair).
- Massage in for 3–5 minutes before rinsing — singing a song can help keep time.
- Rotate 2–3 different shampoos for best results. Common active ingredients:
- Selenium sulfide — controls yeast and helps shed flakes.
- Zinc pyrithione — calms inflammation, controls yeast and bacteria.
- Ketoconazole — antifungal, works against yeast.
- Salicylic acid — loosens flakes, reduces oil.
- Tar or sulfur — calms inflammation (may leave a smell).
- Adjust frequency to hair type and style:
- Oily hair may need daily use during flares.
- Long, curly, coily, or braided hair may need less frequent use.
- Avoid applying hair products to the scalp; keep them on the hair shaft only.
- Take breaks from harsh treatments (chemical relaxers, hot irons, tight extensions) during flares.
Care tips for face and body:
- Medicated shampoos can be used as a gentle wash on affected areas (avoid eyes).
- Over‑the‑counter creams may help:
- Low‑strength cortisone cream for inflammation.
- Antifungal creams (clotrimazole, miconazole) for yeast control.
- For sensitive skin, test a small area first and watch for irritation.
Workshop‑recommended Over-the-Counter Shampoos
(Rotate 2–3 for best results; always follow label directions and check for sensitivities)
Prescription Options (Doctor‑Directed)
If OTC care isn’t enough, a doctor may recommend:
- Ketoconazole 2% shampoo or ciclopirox 1% shampoo (stronger antifungal action).
- Prescription corticosteroid solutions/foams for scalp inflammation (e.g., fluocinolone 0.01%, fluocinonide 0.05%, clobetasol 0.05%) — usually short‑term use.
- Fluocinolone 0.01% oil for sensitive areas or younger patients.
Workshop‑Recommended Face & Body Products
- Antifungal creams: clotrimazole (Lotrimin®), miconazole (Micatin®) — thin layer to rash areas
- Low‑strength hydrocortisone cream (0.5–1%) — short‑term use for redness/itch
- Gentle cleansers: Cetaphil® Gentle Skin Cleanser, Vanicream® Gentle Facial Cleanser — non‑soap, fragrance‑free.
Sensory‑friendly strategies:
- Let your teen/adult choose between shampoo scents or textures when possible.
- Use a handheld mirror so they can see what’s happening during scalp care.
- Turn shampoo time into a predictable routine — same day, same steps each week.
- Offer a towel or cloth to shield the face from drips.
- If they dislike the feel of medicated shampoo, follow with a favorite conditioner on the hair only.
When to call the doctor:
- No improvement after a few weeks of consistent care.
- Rash spreads rapidly, becomes painful, or shows signs of infection (pus, swelling, fever).
- You need to use cortisone creams almost daily to keep symptoms down.
What to expect:
- With treatment, flakes and redness usually improve in days to weeks.
- Temporary light or dark patches may remain after the rash clears — these usually fade in 1–3 months.
- Some people can stop treatment once clear; others need occasional maintenance to prevent flares.
3. Psoriasis
Looks like:
- Red, raised patches with thick white or silvery scales (on darker skin, patches may look dark red, purple, or dark brown).
- Common on elbows, knees, and scalp, but can appear anywhere — including nails (thick, yellow, or pitted).
- May be itchy, sore, or cause a burning sensation.
- Can range from a few small spots to large areas of skin.
- May come and go in unpredictable cycles.
Why it happens:
Psoriasis is an immune‑mediated condition — the immune system mistakenly speeds up the skin cell growth cycle.
- Normal skin cells mature and shed in 3–4 weeks; in psoriasis, this happens in just 3–4 days, causing thick, scaly build‑up.
- Genetics play a role — if a parent has psoriasis, there’s about a 25% chance their child will develop it.
- In people with Down Syndrome, immune system differences (including increased interferon signaling) may contribute to higher rates of psoriasis, especially in adulthood.
- Triggers can cause flare‑ups or make symptoms worse:
- Infections (e.g., strep throat, ear infections, colds) — flares may appear 2–6 weeks later.
- Skin injury (scrapes, cuts, friction) — “Koebner phenomenon”.
- Stress or anxiety.
- Cold, dry weather.
How common in Down Syndrome:
- Around 1% of children and 3% of adults with DS have psoriasis — similar to or slightly higher than the general population.
- Adults with DS are about 4 times more likely to have psoriasis than children with DS.
- More common in men than women with DS.
Health considerations beyond the skin:
- Psoriasis can affect nails and joints (psoriatic arthritis) — watch for joint pain or swelling.
- In adults, psoriasis is linked to higher risk of obesity, diabetes, high cholesterol, and high blood pressure — these risks are lower in children but increase with age.
- Psoriasis can impact self‑esteem, mood, and social comfort — depression and anxiety are more common.
Care tips for mild to moderate psoriasis
Daily skin care:
- Moisturize often — thick creams or ointments help reduce dryness, scaling, and itching.
- Avoid harsh soaps — use gentle, fragrance‑free cleansers.
- Bathe in lukewarm water — short baths/showers; pat skin dry and moisturize immediately.
Managing triggers:
- Treat infections promptly.
- Protect skin from injury — use gloves for chores, avoid scratching.
- Build stress‑reduction into routines (music, movement, prayer, or quiet time).
- Use a humidifier in dry seasons.
Treatment options (doctor‑guided)
There’s no cure, but many treatments can control symptoms. Your dermatologist will tailor the plan to your teen/adult’s needs, location of psoriasis, and severity.
Topical treatments (most common for mild disease):
- Corticosteroid creams/ointments — reduce inflammation and redness.
- Vitamin D analogues (e.g., calcipotriene) — slow skin cell growth.
- Coal tar preparations — reduce scaling and itching.
- Salicylic acid — helps remove scales.
- Calcineurin inhibitors (e.g., tacrolimus) — for sensitive areas like face or skin folds.
Light therapy (phototherapy):
- Controlled exposure to UVB light in a clinic setting — helpful for widespread psoriasis.
Systemic medications (for moderate to severe disease):
- Oral medications — methotrexate, acitretin, cyclosporine.
- Biologic injections — adalimumab, ustekinumab, apremilast, and others.
- These require close monitoring for side effects and are usually prescribed by a dermatologist experienced in treating people with DS.
Sensory‑friendly & independence‑building tips
- Let your teen/adult choose between cream or ointment textures.
- Use a visual schedule for treatment steps.
- Turn moisturizing into a game or creative activity (draw shapes with cream).
- Keep products in a visible, easy‑to‑reach spot to encourage self‑care.
When to call the doctor
- Rapid worsening or spreading of patches.
- Signs of infection (fever, pus, swelling, spreading redness).
- New joint pain or swelling.
- No improvement after several weeks of consistent care.
- If psoriasis is affecting mood, sleep, or daily activities.
What to expect:
- Psoriasis often improves with treatment but can return — ongoing management is common.
- Flare‑ups may be shorter and less severe once a good routine is in place.
- With the right plan, most people can keep symptoms under control and maintain comfort and confidence
4. Alopecia Areata (Autoimmune Hair Loss)
Looks like:
- Sudden, round or oval patches of hair loss on the scalp (skin may look smooth or slightly peach‑fuzzed).
- Can occur anywhere hair grows — eyebrows, eyelashes, beard area, arms, or legs.
- In some cases, all scalp hair is lost (alopecia totalis) or all scalp and body hair (alopecia universalis).
- Nails may show tiny pits, ridges, or roughness.
Why it happens:
Alopecia areata is an autoimmune condition — the immune system mistakenly attacks the hair follicle, causing hair to fall out.
- In people with Down Syndrome, immune system differences (including increased interferon signaling and changes in the AIRE gene on chromosome 21) make autoimmune conditions more common.
- Alopecia areata is much more common in DS: about 0.83% of people with DS vs. 0.06% in the general population — a 15‑fold increase.
- It often appears earlier in life and may be more severe in DS.
- People with DS who have alopecia areata are also more likely to have thyroid disease — regular thyroid screening is important.
Possible triggers:
- Illness or infection
- Significant stress
- Sometimes no clear trigger at all
Health connections caregivers should know:
- Thyroid checks: For people with DS, thyroid function should be checked at 6 months, 12 months, annually from age 1, and every 1–2 years from age 21 — especially if alopecia areata is present.
- Alopecia areata is not contagious and not a sign of cancer.
- Hair often grows back, but the process can take months or years, and new patches can appear.
Treatment options (doctor‑guided)
There’s no cure, but treatments can help hair regrow and reduce new patch formation. Plans are tailored to age, severity, and comfort level.
Topical treatments:
- Topical corticosteroids (creams, ointments, solutions) — reduce inflammation around follicles.
- Topical irritants (e.g., squaric acid, DPCP) — redirect immune activity in the scalp.
- Minoxidil (solution or foam) — increases blood flow to follicles, keeps hairs in growth phase.
- JAK inhibitor creams — newer option for mild cases.
Injections:
- Intralesional corticosteroids — injected into bald patches to calm inflammation (usually for older teens/adults; can be uncomfortable).
Oral treatments:
- JAK inhibitors — for more severe or widespread alopecia; require close monitoring.
- Other systemic medications (e.g., methotrexate, prednisone) — used in select cases.
No‑treatment approach:
- In mild cases, some families choose to watch and wait — spontaneous regrowth is possible.
Sensory‑friendly & independence‑building tips:
- Let your teen/adult choose hats, scarves, or wigs if they want to cover hair loss — or go without if they prefer.
- Practice responses to questions from peers or the public (“I have alopecia — it’s not contagious”).
- Use a mirror and involve them in applying topical treatments to build self‑care skills.
- Keep treatment steps predictable — same time, same place — to reduce anxiety.
- Offer choices in product texture (cream vs. foam) to improve comfort.
Emotional support matters
Hair loss can affect self‑esteem, social comfort, and mood.
- Encourage open conversations about feelings.
- Connect with peer support groups (e.g., In the US, they have National Alopecia Areata Foundation, Children’s Alopecia Project) — even for adults, these can be empowering.
- Involve trusted friends, family, or counselors if needed.
When to call the doctor
- Rapidly spreading hair loss.
- New symptoms like fatigue, weight changes, or mood changes (possible thyroid issues).
- Signs of scalp infection (redness, swelling, pus).
- Interest in exploring prescription treatments.
What to expect:
- Hair regrowth may start as fine, light hairs that thicken and darken over time.
- Alopecia areata can be unpredictable — cycles of loss and regrowth are common.
- Even if hair regrows, ongoing monitoring is important to catch new patches early and check thyroid health.
5. Folliculitis & Hidradenitis Suppurativa (HS)
Folliculitis
Looks like:
- Small, pink or red bumps around hair follicles — may be itchy or sore.
- Sometimes with pus, crusting, or peeling skin.
- Most common on buttocks and thighs, but can appear anywhere hair grows.
- May leave behind dark or pink spots that fade over time.
- A single bump can become a boil (swollen, red, painful lump) or abscess (deeper, pus‑filled swelling).
Why it happens:
- Folliculitis is inflammation or infection of the hair follicle.
- In Down Syndrome, differences in skin proteins and immune function (linked to the extra chromosome 21) may make follicles more prone to blockage and inflammation.
- Friction from clothing, shaving, or sitting for long periods can irritate follicles.
- Blocked follicles can trap bacteria that normally live on the skin, leading to redness, swelling, and bumps.
Prevention tips:
- Wash skin regularly with an antibacterial wash (e.g., benzoyl peroxide, chlorhexidine) — let sit for 3–5 minutes before rinsing.
- Avoid sharing washcloths, towels, or razors.
- Wear loose, breathable clothing; avoid tight fabrics that rub.
- Shaving care:
- Avoid shaving if possible; if needed, use an electric razor.
- Shave in the direction of hair growth with shaving cream to reduce friction.
Treatment options (doctor‑guided):
- Antibacterial washes — benzoyl peroxide, chlorhexidine, sodium hypochlorite, or diluted bleach baths (recipe: ¼ cup bleach in half a tub of water; soak 5–15 min, 2–3 times/week).
- Topical antibiotics — clindamycin, mupirocin, or erythromycin.
- Oral antibiotics — for more severe or widespread cases.
- Drainage — for large boils/abscesses (done by a healthcare provider).
- Oral zinc supplements — sometimes used under medical supervision.
Hidradenitis Suppurativa (HS)
Looks like:
- Painful, deep bumps or abscesses in skin folds (armpits, groin, buttock crease, under breasts).
- May start as blackheads or tender lumps, then progress to draining sores.
- Can form tunnels (“sinus tracts”) under the skin that heal with scarring.
- Drainage may have an odor.
- Can range from mild to severe; often chronic and recurring.
Why it happens:
- HS is not an infection and not contagious.
- In DS, immune system changes and skin structure differences increase HS risk.
- May run in families; can start earlier in people with DS (sometimes before age 10).
- Friction, heat, and hormonal changes can worsen symptoms.
How common in DS:
- General population: ~0.3%
- People with DS: ~2.1% — 7 times more common
- 80% of people with DS who develop HS are diagnosed before age 29 (vs. 34% without DS).
Care & management tips:
- Annual skin checks starting around age 8–10 to catch HS early.
- Wear loose, breathable clothing; avoid close shaving in affected areas.
- Wash gently with antibacterial washes (benzoyl peroxide, chlorhexidine).
- Avoid picking or squeezing bumps — can worsen inflammation and scarring.
- Warm compresses or gentle soaks can help drainage.
- Maintain a healthy weight to reduce skin‑on‑skin friction.
Treatment options (doctor‑guided):
- Topical antibiotics — clindamycin, metronidazole.
- Oral antibiotics — doxycycline, cephalexin (often for weeks to months).
- Hormonal therapy (for females) — certain birth control pills, spironolactone.
- Oral retinoids — isotretinoin, acitretin.
- Biologics — adalimumab (FDA‑approved for HS in ages 12+), infliximab, secukinumab, JAK inhibitors.
- Intralesional corticosteroid injections — to reduce swelling and pain in individual lesions.
- Laser hair removal — may reduce flare‑ups in some cases.
- Surgery — for persistent tunnels or severe disease.
Sensory‑friendly & caregiver strategies
- Involve your teen/adult in choosing cleansers or topical products — texture and scent matter.
- Use visual schedules for wash routines and treatment steps.
- Offer privacy and dignity during skin checks and treatment.
- If injections or laser are needed, ask about numbing creams, distraction tools, or Child Life Specialist support.
- Keep a “skin care kit” with all needed products in one place for consistency.
When to call the doctor
- Rapidly worsening pain, swelling, or redness.
- Fever or signs of spreading infection.
- New drainage with foul odor.
- No improvement after several weeks of consistent care.
- HS symptoms affecting mobility, sleep, or emotional wellbeing.
What to expect:
- Both folliculitis and HS can be long‑term conditions, but early, consistent care can reduce flares, prevent complications, and improve comfort.
- In HS, treatment often focuses on controlling symptoms and preventing new lesions rather than “curing” the condition.
- Emotional support is as important as physical care — these conditions can impact self‑esteem and social confidence.
6. Fungal Infections (Tinea, Athlete’s Foot, Nail Fungus)
Looks like:
- On skin (tinea corporis, faciei, cruris): Red, scaly ring with a clear center; may be one ring or several overlapping; edges are often raised and more inflamed than the center.
- On scalp (tinea capitis): Flaky skin like dandruff, sometimes with pus bumps, hair breakage, or smooth bald patches; may have redness, crusting, or swelling; nearby lymph nodes in the neck may be enlarged.
- On feet (tinea pedis / “athlete’s foot”): Moist, flaky skin between toes; sometimes red, scaly rings on top of toes or feet; peeling or thickened skin on soles; occasional blisters.
- On nails (onychomycosis): Thick, yellow, brittle nails with buildup under the nail edge; more common in adults but can occur in teens, especially if a household member has it.
Why it happens:
- Caused by fungi (dermatophytes) that live on skin, hair, and nails.
- People with Down Syndrome may be more prone due to immune system differences and skin barrier changes.
- Fungi thrive in warm, moist environments — skin folds, sweaty shoes, damp clothing.
- Highly contagious — spreads through direct skin contact, shared items (combs, hats, towels), contaminated surfaces (locker rooms, gym mats, pool decks), soil, or pets.
Prevention tips for family caregivers:
- Avoid sharing combs, brushes, hats, pillowcases, towels, or shoes.
- Keep combs and brushes clean; disinfect regularly.
- Towel dry thoroughly after bathing, especially between toes and in skin folds.
- Wear sandals or flip‑flops in public showers, locker rooms, and pool areas.
- Change socks at least once daily; choose breathable, moisture‑wicking fabrics.
- Keep shoes dry — alternate pairs to allow drying time; consider antifungal powders.
- For scalp infections in the household, all close contacts may need medicated shampoo to prevent spread.
Treatment options (doctor‑guided)
For skin (body, face, groin, feet):
- Topical antifungals — creams, lotions, gels, or sprays applied 1–2 times daily for 2–4 weeks.
- OTC examples: terbinafine 1% (Lamisil®), clotrimazole 1% (Lotrimin®), miconazole 2% (Micatin®), tolnaftate (Tinactin®).
- Prescription examples: ketoconazole 2%, ciclopirox 0.77–1%, oxiconazole 1%.
- Continue treatment for at least 1 week after rash clears to prevent recurrence.
For scalp (tinea capitis):
- Oral antifungals — griseofulvin, terbinafine, fluconazole, or itraconazole for several weeks to months.
- Medicated shampoo (ketoconazole 2% or selenium sulfide 1–2.5%) 2–3 times/week for the person with infection and household contacts — helps reduce spread but won’t cure on its own.
For nails (onychomycosis):
- Oral antifungals — terbinafine or itraconazole for 1–3 months (fingernails) or 3–6 months (toenails).
- Topical nail treatments — ciclopirox lacquer, efinaconazole solution; often better tolerated in children/teens.
- Nail infections are slow to clear — visible improvement may take 6–12 months.
Sensory‑friendly & independence‑building tips:
- Let your teen/adult choose between cream, gel, or spray forms for comfort.
- Use a mirror for self‑application on visible areas; caregivers can assist with hard‑to‑reach spots.
- Make treatment part of a predictable daily routine — e.g., after tooth‑brushing or before bed.
- For scalp shampoo, use a timer or song to make the “leave‑on” time easier to tolerate.
- Keep a dedicated “fungal care kit” with product, towel, and comb to avoid cross‑contamination.
When to call the doctor
- Rash spreads quickly or worsens despite OTC treatment.
- Scalp involvement (always needs prescription oral medication).
- Nail changes that are painful, spreading, or causing difficulty with daily activities.
- Signs of bacterial infection — pus, swelling, fever.
- Recurring infections despite good hygiene and treatment.
What to expect:
- Skin infections often improve within 1–2 weeks of starting treatment; nails and scalp take longer.
- Even after clearing, reinfection is common if preventive steps aren’t followed.
- With consistent care, most fungal infections can be fully cleared and kept from coming back.
Partnering With Professionals
This article is not a substitute for professional advice. Speaking with your doctor is of utmost importance to ensure that your loved one’s skin conditions are diagnosed properly. Therefore:
- Take photos of skin changes to show your doctor.
- If you can’t find a brand, ask for the active ingredient so you can locate a local equivalent.
- Small problems are easier (and less costly) to solve than big ones.
At the workshop, Dr. Rork also shared a valuable set of free skin care handouts created in partnership between the Society for Pediatric Dermatology (SPD) and the LuMind IDSC Foundation. These guides use simple language and clear photographs to help families recognize and manage common skin conditions in people with Down Syndrome — including the Big 6 above.
They are available to anyone, anywhere, at: https://pedsderm.net/for-patients-families/resources-for-patients-with-down-syndrome/. If clicking links isn’t easy where you are, search online for “Down syndrome skin handouts” and look for the SPD link. Please download, print, and share them widely — they are a gift of knowledge that can travel across borders and truly make a difference.
Quick Reference: The Big 6 Skin Concerns & Recommended Products
Feel free to download this quick reference guide.
A Word From My Heart to Yours
Caring for someone with Down Syndrome is a journey of courage, patience, and deep love. We face hard days — but moments like these, when we can take an action that brings relief and joy quickly, remind us that we are making a difference.
You are not alone in this. The HappyDowns community is here to share not just knowledge, but encouragement.
Your love is seen. Your work matters. And your loved one’s comfort is worth every effort.